Getting Started with the Claims Page
The Claims Page is where you manage your billing workflow in Insights. It centralizes claim review, validation, assignment, and submission in one interface, helping you process claims faster and catch errors before they become rejections.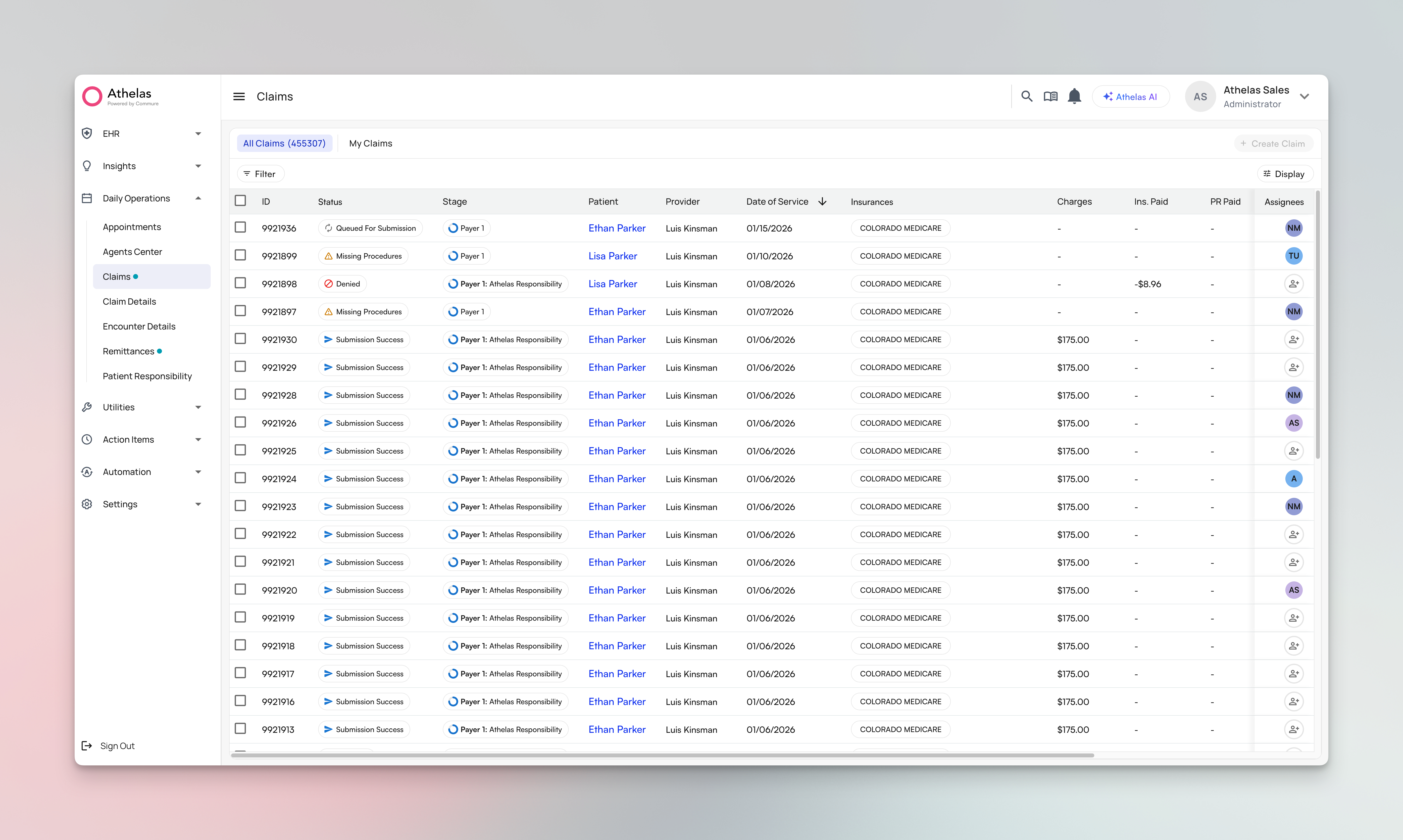
We’re transitioning from “encounters” to “claims” terminology to better match industry standards—the underlying data remains the same.
What is the Claims Page?
The Claims Page gives you a unified view of all claims requiring review or action. You can filter claims by status, insurance, or age, assign work to team members, review AI validation flags, and submit claims—all without switching between tools. Key capabilities:- Filter and save views to focus on specific claim types, providers, or deadlines
- Assign claims individually or in bulk to balance team workload
- Review AI validation that flags errors and suggests corrections before submission
- Collaborate with your team through comments and activity tracking (coming soon)
- Submit with the correct form - Claims automatically generate in the appropriate format (CMS-1500, UB-04, or ADA) based on the selected payer(s)
Getting Started
Accessing the Claims Page
Log in to Insights at insights.athelas.com and navigate to Claims from the Daily Operations tab. The page opens with your most recent view, or a default table showing all active claims.
Working with Claims
Organizing Your Workflow with Filters
- Apply filters that match your workflow (e.g., filter for claims older than 85 days with status “Ready to Submit”)
- Sort by the column that matters most (typically date of service for timely filing)
- Click Save View and name it (e.g., “In Progress”)
- Click ‘Save’ button one more time and the saved view will appears in the view dropdown
Custom views are personal by default, meaning your saved views won’t be seen by anyone else.
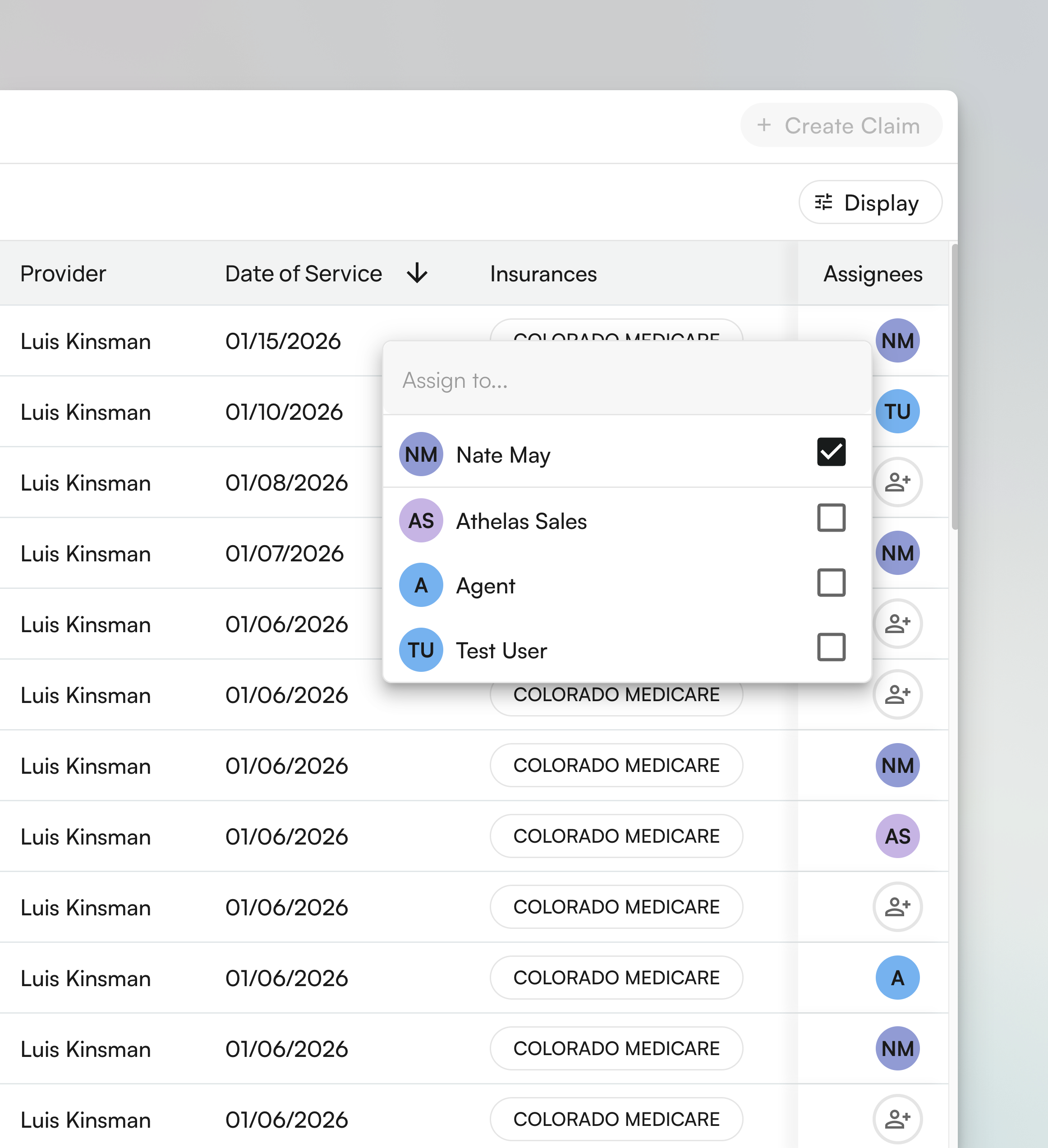
Assigning Claims to Your Team
- Single claim: Click the claim row, then select a team member from the Assigned To dropdown in the detail view
- Bulk assignment: Select multiple claims using checkboxes, then click Bulk Actions > Assign and choose the team member
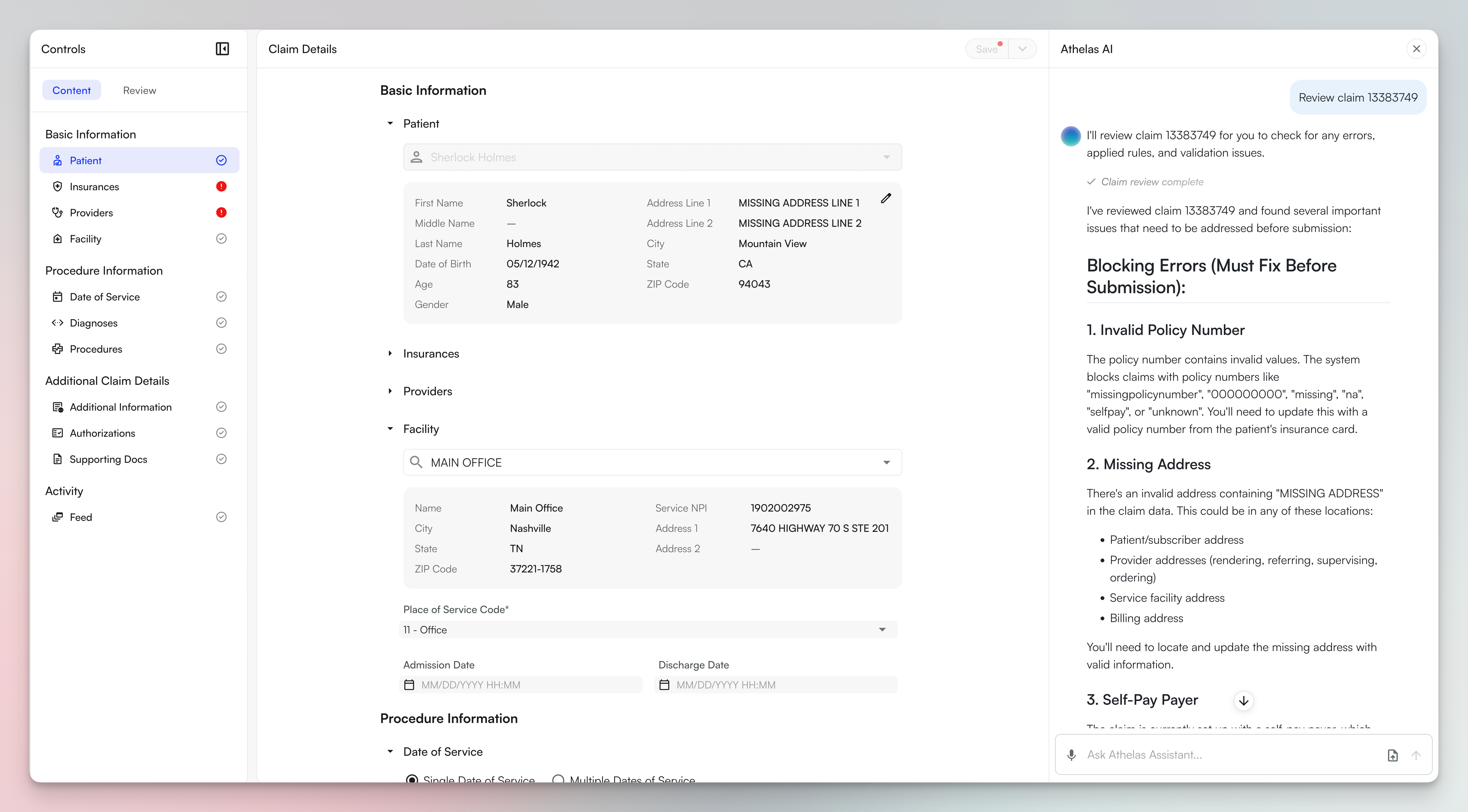
Reviewing Claims with AI Validation
Collaborating Through Comments
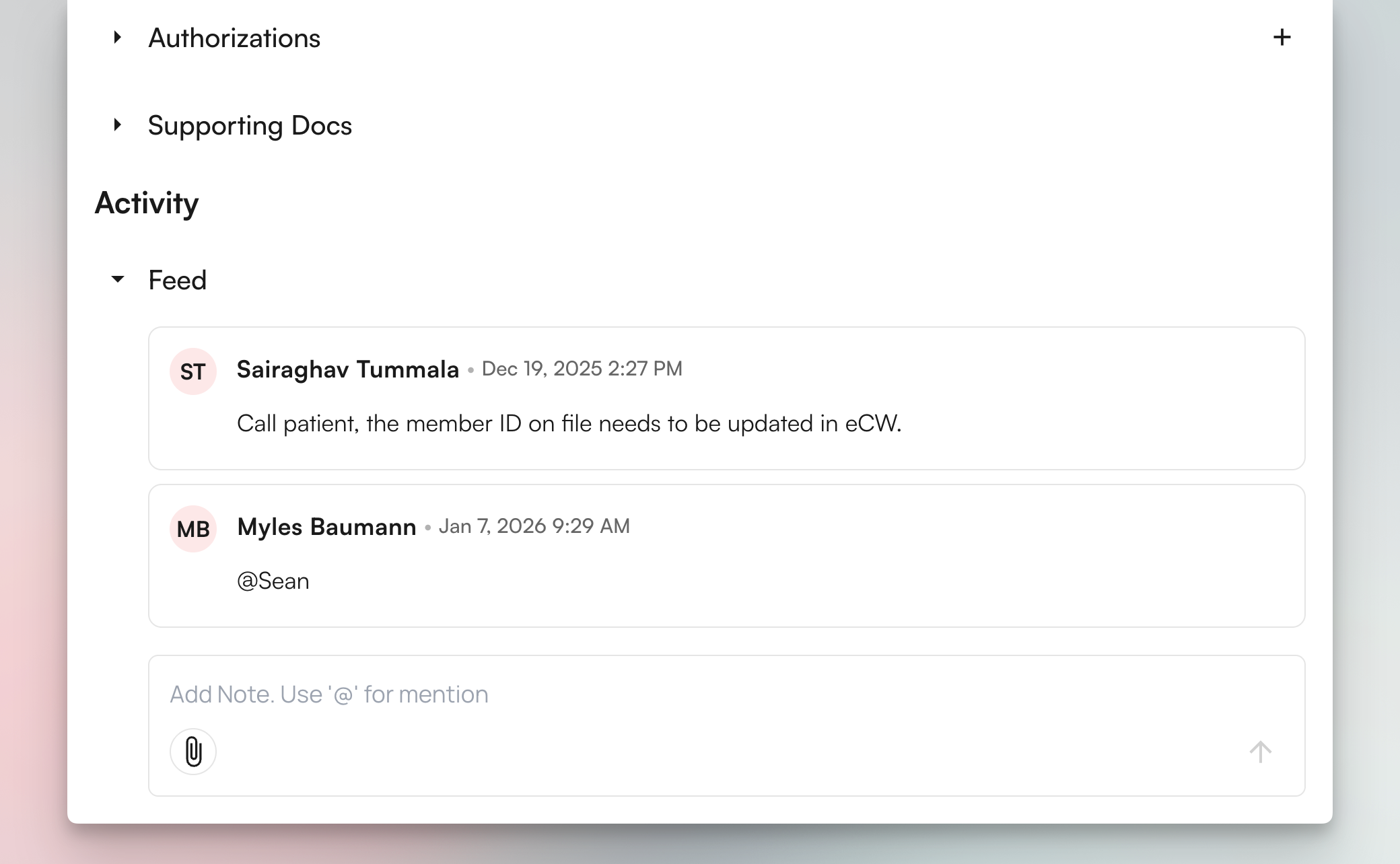
- Leave context for the next person who reviews the claim
- Use @mentions to notify specific team members (e.g., “@Sarah can you verify this diagnosis code?”)
- Check the feed before working on a claim to see if someone already identified issues
Submitting Claims
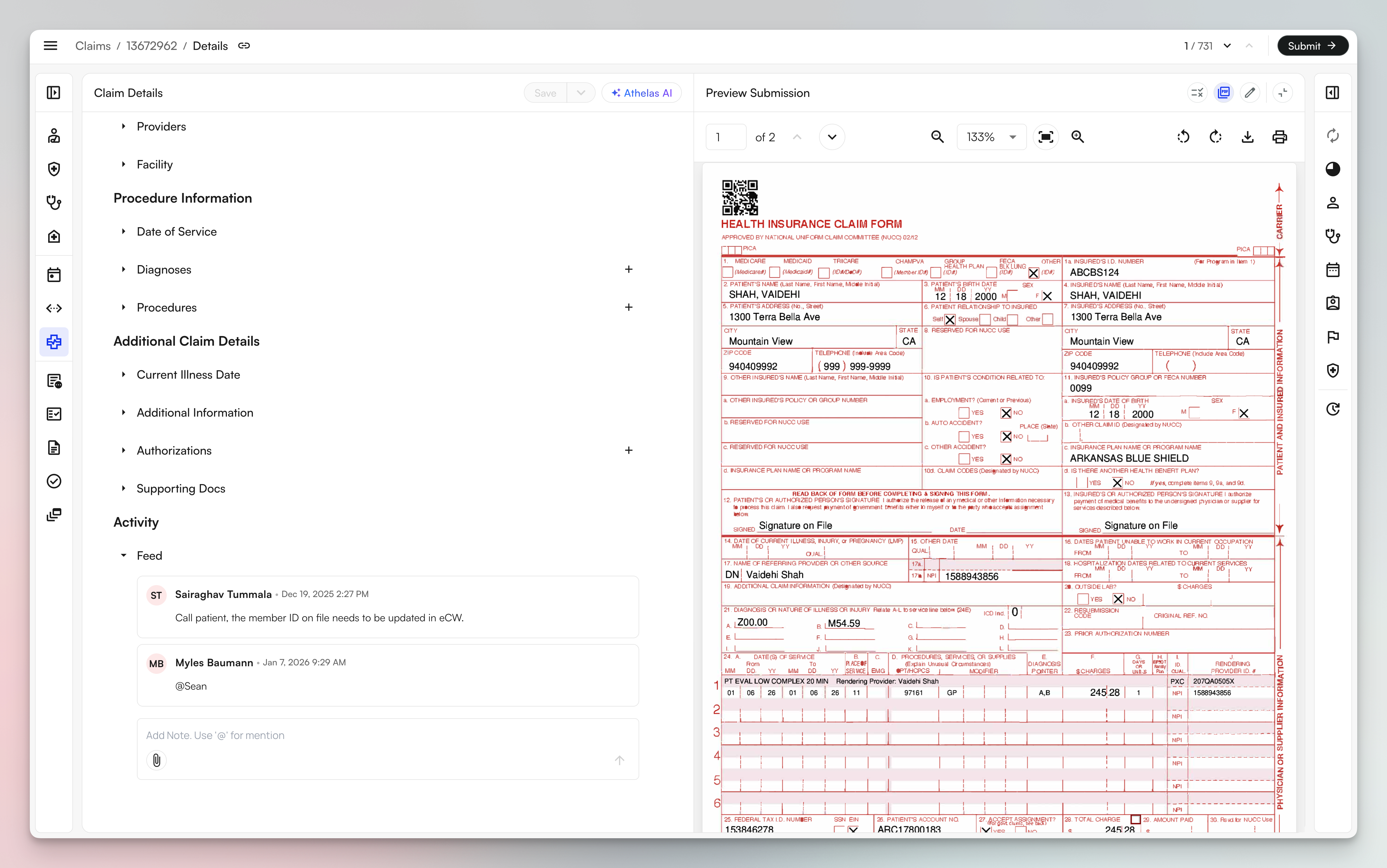
- Review the claim in the Claim Details panel on the left - this shows all your claim data fields
- Click Preview Submission to see the formatted form (CMS-1500, UB-04, or ADA) on the right
- The preview displays exactly how the claim will appear when submitted to the payer
- Work with both views open to verify your claim data translates correctly to the final format
- Make changes to the claim as needed - when you edit claim fields, the preview becomes semi-transparent and shows “Not Synced” to indicate it needs to be refreshed. This occurs because the submission hasn’t run through billing rules since your last update, making the preview stale relative to the current claim state.
- Save your edits to the claim to refresh the preview and see your changes reflected in the formatted submission
- Review the Claim Details panel to confirm all fields are correct
- Click Preview PDF to see the formatted CMS-1500, UB-04, or ADA form exactly as it will submit
- Click the pencil icon in the submission preview to edit specific fields
- These edits only affect this submission and don’t change the underlying claim data
- Review patient, insurance, diagnosis, and procedure information one final time
- Click Submit when ready
- The claim moves to “Submitted” status and appears in your submission history
FAQ
How do I know if a claim is ready to submit?
How do I know if a claim is ready to submit?
Review the AI validation flags in the Claim Details panel. Claims are ready to submit when:
- All required fields are filled in
- No critical validation errors are present (red indicators)
- The preview submission shows the correct format for your payer
- Patient, insurance, diagnosis, and procedure information is accurate
What's the difference between editing the claim and editing the submission directly?
What's the difference between editing the claim and editing the submission directly?
When you edit the claim in the Claim Details panel, your changes go through billing rules and update the underlying claim data. This ensures consistency and proper rule application.When you edit the submission directly (using the pencil icon in the preview), your changes bypass billing rules and only affect that specific submission output. The underlying claim data remains unchanged.Note: Direct submission edits should be used sparingly for final adjustments only, as they don’t go through the normal billing rules engine.
Can I share my saved views with other team members?
Can I share my saved views with other team members?
What happens if I need to make changes after submitting a claim?
What happens if I need to make changes after submitting a claim?
Once a claim moves to “Submitted” status, you’ll need to work with your billing team to make adjustments. The claim will appear in your submission history, and you may need to resubmit or make corrections depending on your practice’s workflow.
How do I filter claims by multiple criteria at once?
How do I filter claims by multiple criteria at once?
Use the filter bar at the top of the table to apply multiple filters simultaneously. You can combine filters for status, insurance provider, claim amount, age, assigned team member, provider, and date range. Once you’ve set up your ideal filter combination, save it as a custom view for quick access later.
